The Infection Prevention and Control Team have identified or developed a large number of useful resources related to Infection Prevention, which we will begin publishing here shortly. We would welcome your feedback on any resources that you require. Please get in touch with us using our team email, hiowicb-hsi.infectionprevention@nhs.net.
Clostridioides difficile Infection
Hampshire and Isle of Wight Integrated Care Board (HIOW ICB) is looking to support management of Clostridioides difficile Infection (CDI) in the community to provide information and support. We recognise that patients who suffer a CDI may frequently have severe and complex underlying co-morbidities and at times it is becoming increasingly difficult to manage as community case, the HIOW ICB would like to extend the offer of clinical support and signposting if you feel this is appropriate.
We have pulled together several resources and links to useful documents to support the management, to minimise the risk of Clostridioides difficile infection and possible onward transmission.
Main action points to reduce risk of infection:
What is Diarrhoea acute/chronic:
- Diarrhoea is the passage of three or more loose or liquid stools per day (or more frequently than is normal for the individual)
- Acute diarrhoea is defined as lasting less than 14 days
- Persistent diarrhoea is defined as lasting more than 14 days
- Chronic diarrhoea is defined as lasting for more than 4 weeks
- Acute diarrhoea is usually caused by a bacterial or viral infection. Other causes include medication, anxiety, food allergy, and acute appendicitis
- Causes of chronic diarrhoea include irritable bowel syndrome, diet, inflammatory bowel disease, coeliac disease, and bowel cancer
- Diarrhoea is one of the most common symptoms for which people seek medical advice
Diarrhoea - adult's assessment | Health topics A to Z | CKS | NICE
What is Clostridioides difficile?
Clostridioides difficile (C. difficile) is a bacterium that’s found in people’s intestines. It can be found in healthy people, where it causes no symptoms (up to 3% of adults and 66% of babies).
C. difficile causes disease when the normal bacteria in the gut are disadvantaged, usually by someone taking antibiotics. This allows C. difficile to grow to unusually high levels. It also allows the toxin that some strains of C. difficile produce to reach levels where it attacks the intestines and causes mild to severe diarrhoea.
C. difficile can lead to more serious infections of the intestines with severe inflammation of the bowel (pseudomembranous colitis). C. difficile is the biggest cause of infectious diarrhoea in hospitalised patients.
You can become infected with C. difficile if you ingest the bacterium (through contact with a contaminated environment or person). People who become infected with C. difficile are usually those who’ve taken antibiotics, particularly the elderly and people whose immune systems are compromised.
Clostridium difficile guidance data and analysis
NHS Patient leaflet c-difficile
Who do you need to test for Clostridioides difficile?
- (Page 13) Department of Health - Updated Guidance on the Diagnosis and Reporting of Clostridium Difficile (2012) DH Title (publishing.service.gov.uk)
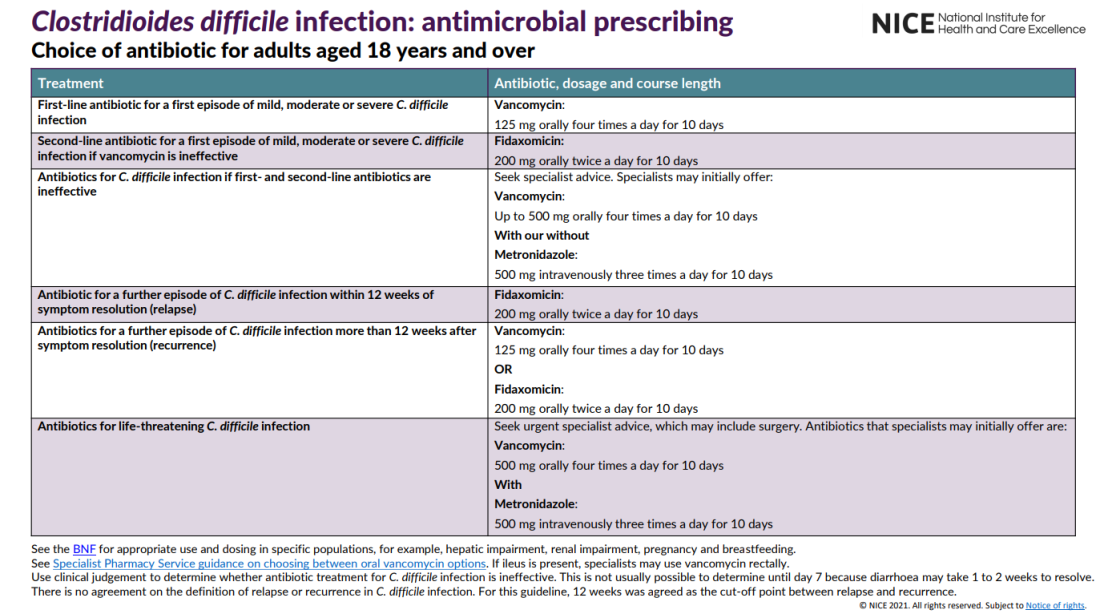
Antimicrobial Prescribing:
- Present guidance is from National Institute for Health and Care Excellence (NICE) 2021.
Overview | Clostridioides difficile infection: antimicrobial prescribing | Guidance | NICE
NG199 visual summary (nice.org.uk)
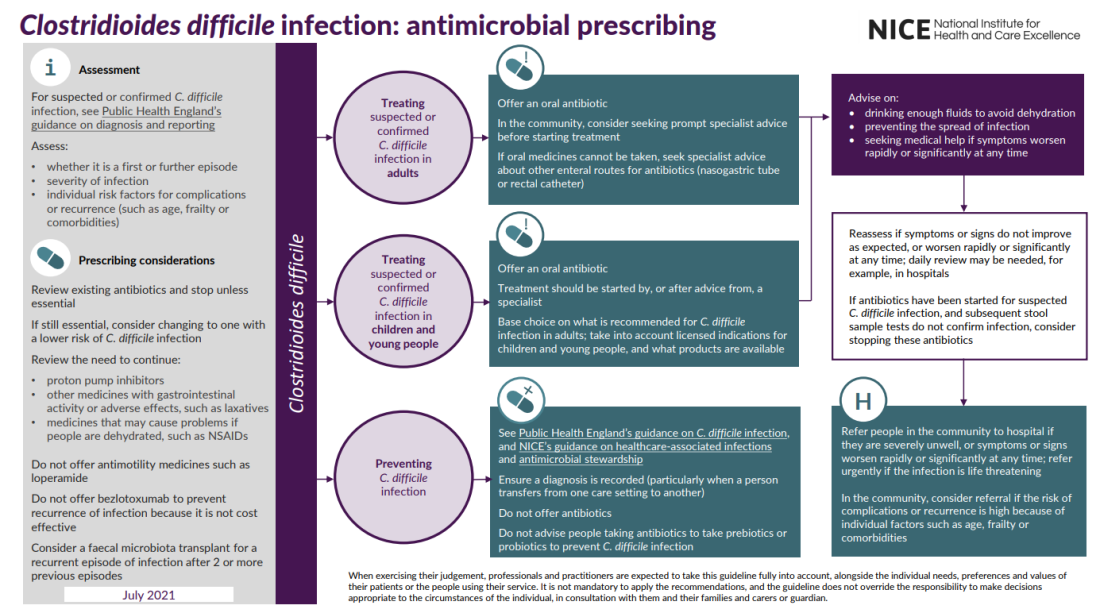
Prescribing considerations, please review existing:
- Antibiotics and stop unless essential If still essential, consider changing to one with a lower risk of C. difficile infection Review the need to continue.
- Proton pump inhibitors (PPI)
- Other medicines with gastrointestinal activity or adverse effects, such as laxatives
- Medicines that may cause problems if people are dehydrated, such as NSAIDs.
- Do not offer antimotility medicines such as loperamide.
- Do not offer Bezlotoxumab to prevent recurrence of infection because it is not cost effective. Bezlotoxumab | Drugs | BNF | NICE
- Consider a faecal microbiota transplant FMT for a recurrent episode of infection after 2 or more previous episodes
When should a known positive be retested?
- Laboratories will not retest a stool sample within 28 days of a previous positive Clostridioides difficile infection CDI.
- Once 28 days has elapsed retesting in patients with recurrent symptoms where symptoms stopped and have reoccurred or where symptoms have changed may be useful.
- Where symptoms are unchanged and have continued, consider treating as per NICE Guidance for further episodes within 12 weeks and/or get specialist advice.
- Where patient has suffered 2 or more (recurrent) episodes of CDI they may be considered for faecal microbiota transplant FMT. NICE recommends transplant with good bacteria taken from poo to resolve recurrent Clostridium difficile infections
Who can I contact if I need more information and support (Health professionals only):
Please contact your local trusts microbiologists if you require advice on whether a repeat sample is required or what treatment options are available and appropriate.
- Hampshire Hospitals NHS Foundation Trust via switchboard 01962 863 535
- Portsmouth Hospitals NHS Trust via switchboard 02392 286 000
- University Hospitals Southampton NHS Foundation Trust via switchboard 02380 777 222
- St Mary Hospital NHS Trust Tel via switchboard 01983 524 081
Useful links and resources:
Infection Prevention Control, You're in safe hands
C. difficile (Clostridioides difficile) Policy for General Practice - Infection Prevention Control
C. difficile (Clostridioides difficile) Policy for Care Home settings - Infection Prevention Control
Recent updates:
Measles: Frequently Asked Questions Version 2.0 April 2024 (NHS England)
We have pulled together a number of resources and links to useful documents to support you with actions required, to minimise the risk of measles transmission within your practices
Main actions points to reduce the risk of transmission:
Risk Assessments:
Measles is a highly transmissible virus, a local risk assessment will support you in identifying areas requiring action see Appendix 1: Practical steps towards completing a local risk assessment for measles in healthcare settings for a risk assessment template
The following sections are priority actions to reduce the risk within your provider setting:
Staff:
• Please ensure you have completed your assessment of all staff vaccination status with regards to MMR
• Any Staff member identified that do not have documented evidence (individual measles vaccine x 2 or MMR x 2 or blood test prooving immunity) to be advised to have MMR X2 via their own GP
Time limited 31 March 2024 On behalf of Jane Freeguard, Deputy Director of Vaccination – Medicines & Pharmacy, NHS England
In light of the national measles outbreak and urgency to support rapid uptake of the MMR vaccine, we are permitting practices to administer MMR vaccines to their eligible staff who are registered with another practice under INT (immediately necessary treatment).Please note this is a time limited arrangement until 31 March 2024 in light of the on-going national incident and only applies to MMR vaccinations.
An item of service fee cannot be claimed for the administration of MMR vaccines to staff registered with another practice. However, indemnity cover will be provided through CNSGP and nationally supplied MMR stock can be used to vaccinate eligible staff.Staff must be strongly encouraged to inform their registered practice that they have received an MMR vaccine, requesting it be included in their medical record.
• Please be aware that Health care workers who are exposed to a confirmed or suspected case of measles and do not have satisfactory evidence of protection (2 documented doses of measles containing vaccine or measles IgG positive) should be excluded from work from the 5th day after their first exposure to 21 days after the final exposure.
• Please see section 2:6 of the NHS England » Guidance for risk assessment and infection prevention and control measures for measles in healthcare settings guidance
Robust Triage:
• Robust triage is an essential part of minimising the exposure risk, of potentially infectious patients.
• All staff undertaking a reception and triage role, should be trained and fully aware of the questions, to be asked when talking to patients requesting an appointment, especially those who report, Fever, Coryza or cough, conjunctivitis and Rash – Please note that some symptoms are experienced before the rash appears but are still infectious.
• Please see Appendix 2 of the NHS England » Guidance for risk assessment and infection prevention and control measures for measles in healthcare settings and NHS England » Measles guidance for primary, community care, emergency departments and hospital
social media materials which may support identification of potenatial measles cases social media resources asking parents to call ahead if they think their child has measles
Isolation Room -Patient Placement:
• If remote consultation is not possible, or if, following telephone triage the patient is advised to attend your primary care setting, please ensure a separate entry area and uncluttered consulting room with a window can be used (if possible) as this allows for minimal transmission within your practice and for the area to be ventilated and all surfaces cleaned following the visit.
• Please note: If your practice has air conditioning and the air is re-circulated you should also turn this off during the visit, again to reduce risk.
• Please see section 2.2.1 of NHS England » Guidance for risk assessment and infection prevention and control measures for measles in healthcare settings
Unvaccinated/Partially vaccinated patients:
• Please ensure patients visiting your practice have their immunisation status checked and offered MMR if appropriate – ‘Every Contact Counts’
Infection Prevention and Control:
• Please ensure all staff are aware of Chapters 1 and 2 of the National Infection Prevention Control Manual as they should all follow the principle regarding Standard Infection control precautions and transmission-based precautions. NHS England » National infection prevention and control. Please see section 2 NHS England » Guidance for risk assessment and infection prevention and control measures for measles in healthcare settings
Person Protective Equipment:
• Please ensure all staff undertaking any procedure should assess any likely exposure.
• Please see Section 2.3 NHS England » Guidance for risk assessment and infection prevention and control measures for measles in healthcare settings and Measles FAQ at the top of this resource page
Referral to Secondary Care:
• Should a patient require transferring to Hospital or ED please inform the Ambulance service and admitting area (if using this them to transfer patient) the patient is being taken too to ensure the appropriate actions and isolation facilities are available when the patient arrives.
• Please see Appendix 2 NHS England » Guidance for risk assessment and infection prevention and control measures for measles in healthcare settings
Suspect Measles
Please call your local health protection team urgently so they can undertake an prompt risk assessment of contacts, to identify vulnerable contacts. UKHSA - HIOW Health Protection team Telephone: 0344 225 3861 or Out of hours urgent enquiries: 0844 967 0082 (please note from 11 March 2024 the in hours number will be for both in and out of hours)
Notifiable diseases: form for registered medical practitioners - GOV.UK (www.gov.uk)
The following resources will support you in ensuring you have robust measures in place to prevent Measles transmission within your setting and to swiftly identify and respond to potential measles case.
National Guidance:
NHS England » Measles guidance for primary, community care, emergency departments and hospital
National measles guidelines January 2024 (publishing.service.gov.uk)
Information on measles for health professionals - GOV.UK (www.gov.uk)
Notifiable diseases and causative organisms: how to report - GOV.UK (www.gov.uk)
Staff member education:
Useful policy templates:
Template policy for placement and isolation of potential or confirmed infectious patient Patient placement (infectionpreventioncontrol.co.uk)
Template policy for Notifiable disease Notifiable diseases (infectionpreventioncontrol.co.uk)
Healthcare staff vaccination:
Healthcare staff immunisation - Immunisation of healthcare and laboratory staff: the green book, chapter 12 - GOV.UK (www.gov.uk)
CQC guidance on primary care staff vaccination GP mythbuster 37: Immunising healthcare staff - Care Quality Commission (cqc.org.uk)
Patient leaflets and social media resources:
- UKHSA MMR and Measles Programme publications and resources
- I think I have got Measles - Call ahead poster
- MMR Leaflet MMR for all leaflet – now available to order in English, Bengali, Polish, Romanian, Somali, Ukrainian and Yoruba
- Video of Consultant Epidemiologist at UKHSA, Dr Colin Campbell
- Video: UKHSA Measles signs and symptoms
- Measles - NHS (www.nhs.uk)
- Measles :: Healthier Together (what0-18.nhs.uk)
- Childhood Vaccinations - Essential information :: Healthier Together (what0-18.nhs.uk)
- Childhood Vaccination 2022 | Help Us Help You - Vaccinations | Campaign Resource Centre (dhsc.gov.uk)
Scabies is a Parasite which burrows into the skin of humans. Symptoms of infection can appear as late as 6-8 weeks post infection, however infected persons can infect others via prolonged skin to skin contact while asymptomatic. Diagnosis can be difficult due to the small lines caused by the burrows being easily destroyed by scratching. For these reasons scabies can be associated with health Care outbreaks.
If you suspect a Scabies Outbreak please contact UKHSA: Telephone (Mon-Fri 9am-5pm): 0344 225 3861; Out-of-hours telephone (Mon-Fri 5pm-9am, Saturday and Sunday): 0844 967 0082
Email address (Mon-Fri 9am-5pm): SE.AcuteResponse@ukhsa.gov.uk
You can also contact the ICB Infection Prevention and Control team on 08703156601 (9am - 4pm, Mon-Fri) hiowicb-hsi.infectionprevention@nhs.net
National Guidnace:
National Institute of Clinical Excellence (NICE) guidance on Scabies
Treatment Guidance:
South Central Antimicrobial Network Scabies prescribing guidance
Template policies, action plan and patient leaflets:
Infection Prevention Control You're In Safe Hands Scabies policy for Care Homes
Infection Prevention Control You're In Safe Hands Scabies policy for Primary Care
Infection Prevention Control You're in Safe hands Scabies policy for Domiciliary care
Infection Prevention Control You're in Safe Hands Scabies treatment patient leaflet