Hampshire and Isle of Wight Integrated Care System has a long history of working together with local partners to enable people in our communities to live healthier, longer lives. By working in partnership, we can provide more consistency of care, break down barriers between services and reduce inequalities.
Addressing these inequalities is a priority that runs throughout our Integrated Care System strategy. Our aim is to provide care that is tailored to individual needs, delivered at the right time and in the right place.
We are delivering on a number of projects to tackle health inequalities across Hampshire and Isle of Wight, which helps us to achieve the four overarching aims of all Integrated Care Systems set by NHS England. These are:
- improve outcomes in population health and healthcare
- tackle inequalities in outcomes, experience and access
- enhance productivity and value for money
- help the NHS support broader social and economic development
By transforming how we engage and support people living with multiple disadvantages, we can include and treat people equally and fairly in a more person-led way.
What do health inequalities look like in...
To help us to identify the health inequalities in our four places (Hampshire, Isle of Wight, Southampton and Portsmouth), we have produced four Joint Strategic Needs Assessments (JSNA). These assessments tell us that across Hampshire and Isle of Wight an ageing population, with increasing frailty and health issues, is one of the biggest drivers in health and social care needs.
We also know that overall, diversity is increasing, but within Isle of Wight and Hampshire we see less ethnically diverse populations than England. This is in contrast to Southampton and Portsmouth where the proportion of ethnic populations is similar to England.
Healthy life expectancy has decreased which means while people are living longer, they are living longer with poor health, and this is particularly true for women and people living in the most deprived areas. The biggest life expectancy gap, between those people who live in the poorer areas and those who live in the wealthier areas, are from deaths caused by circulatory diseases, cancer and respiratory diseases.
In terms of preventable deaths, cancers are the biggest cause across the area, where 50 per cent of the cancers are considered preventable. Cardiovascular diseases have the second highest number of preventable deaths. Smoking, high blood sugars and high body mass index drive most of the death and disability across the whole population.
Vulnerable coastal and left behind neighbourhoods have been identified across Hampshire and Isle of Wight area and recognised as experiencing more ill health, particularly heart disease, diabetes, cancer, and mental health. These areas also have high rates of unemployment, high rates of obesity and life expectancy is lower.
Across Portsmouth there are some very stark health inequalities, which mean that in the most deprived areas of the city, men will live 15 years shorter, compared with the least deprived areas.
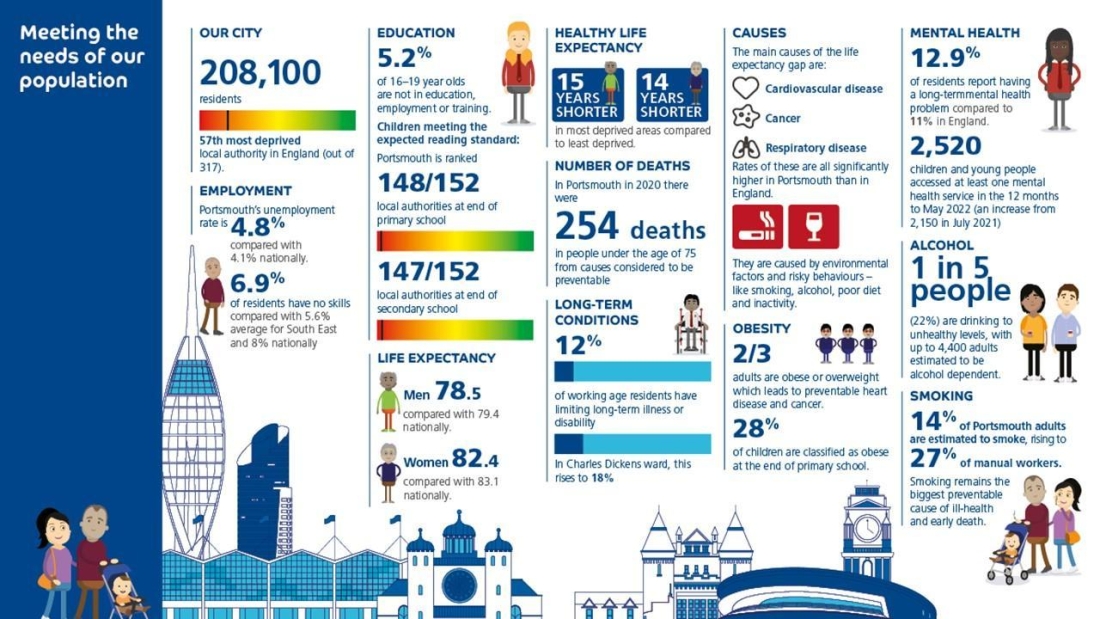
That’s a big difference and that’s just one of the many health inequality issues faced by the city. Preventable health conditions caused by smoking, alcohol, poor diet, and lack of exercise, are among the main causes of this lower healthy life expectancy.
Portsmouth is ranked 57th most deprived authority in England out of 317 areas. 13% of Portsmouth’s population live in the 10% most deprived areas nationally and over 60% are in the most deprived two quintiles.
Of households in Portsmouth 25% live in relative poverty. In 2019/20 17% of children were in absolute low-income families (before housing costs). This varies from 29% of children in the most deprived ward to 7% of children in the least deprived ward.
All of these issues have worsened during the pandemic and cost of living crisis. Health and care teams across the city are working with voluntary sector partners to reach out to those residents who need better access to support to live healthier lives.
There is a lot of excellent work taking place to support Portsmouth residents to live healthier lives, including two projects which were started during the pandemic, to try to reach more communities to encourage vaccine uptake – which are now being used to support those same communities with health and wellbeing issues.
Live Well Sessions
Live Well sessions were started initially to improve the uptake of Covid-19 vaccines in the most deprived areas of Portsmouth, but these have now been developed into a whole series of health and wellbeing support sessions.
The sessions are delivered at places where people are already meeting, so the teams will attend local food banks, and then talk to people who come in for food, about all the support available for other aspects of their lives.
The Live Well sessions are designed to make it easier for local communities to access health and care services, by taking them out to people. This is particularly important in those communities where people might not have easy access to services for a number of reasons.
It’s a completely collaborative effort with the council team working with the food banks, community pantries and larders, to bring health and care services along to offer a wide range of support, including:
- primary care networks
- social prescribers
- Solent Mind and Talking Change (IAPT service)
- a variety of services offering support to those with cost of living needs
- Portsmouth wellbeing team - healthy eating, stopping smoking and weight management
- local partners who are delivering blood pressure checks
- Hive Portsmouth providing knowledge and awareness of local support for a number of issues, including their very own uniform shop
Community Champions
The community champions programme started during the pandemic, to better understand the reluctance of some communities to take up the vaccine. Now, these same champions are offering insight into communities who are struggling with health, wellbeing cost of living issues instead.
For example, the menopause was identified by one community champion where accessible information and awareness was needed. Subsequently messages have been created and shared, a community resource has been established at a local library and workshops and training are in development.
These are just two examples of the important work being carried out every day by health and care teams working together across Portsmouth, to help tackle health inequalities and to support people from all communities to live a healthier, happier and longer life across the city.
Many health outcomes in Southampton remain below regional and national average. Within the city, inequalities in the conditions in which people are born, grow, live, work and age lead to further unfair and avoidable different experiences of health and wellbeing.
Southampton’s overall life expectancy at birth is lower than the England average and shows signs of falling, if this continues it means that children born in Southampton are expected to die at a younger average age than those born elsewhere in the country or those born several years ago.
Within the city, the gap in average life expectancy between the most and least deprived areas is almost nine years for males and four years for females. This means that males born in the most deprived parts of the city have a life expectancy nine years lower than those born in the most affluent areas and women born in the most deprived parts, four years lower than those born in the most affluent.
Not only more do people living in the most deprived parts of the city die earlier than those in the most affluent, but they also experience long-term conditions earlier and have worse average outcomes throughout life.
Work to date across Southampton has highlighted clear policy areas for action to reduce health inequalities, covering the whole of life and wider determinants of health:
- Give every child the best start in life
- Enable all children, young people and adults to maximise their capabilities and have control over their lives
- Create fair employment and good work for all
- Ensure a healthy standard of living for all
- Create and develop healthy and sustainable places and communities
- Strengthen the role and impact of ill-health prevention
Innovative work and projects are already taking place across the city in all six of these areas, to help improve the health and wellbeing of everyone living in Southampton.
Re:Minds:
This is a Southampton-based organisation supporting families whose children and young people have autism, ADHD or other neurodiverse needs and/or mental health needs. They provide opportunities for parents to share knowledge, experiences and challenges and they reduce isolation and give support through their core offer of regular group sessions, advice clinics, 1:1 support and representing families.
Through developing trusting relationships with key services and organisations, such as Children and Adult Mental Health Services, Re:Minds have been able to work in partnership to address the varied needs of families who access their support. Starting from a first meeting with 12 attendees, Re:Minds now has over 2200 members and is staffed by a 7 members of staff and volunteers.
Crops in Pots:
This project aimed to encourage learners to engage in practical horticultural skills on their doorstep, learning both what plants to grow and how they contribute to the wider environment. Three weekly ‘Crops in Pots’ sessions were held at Moorlands Community Centre with the aim of teaching learners how to grow veg, herbs and both companion plants and plants for pollinators -in small spaces, pots, balconies and windowsills, using recycled milk bottles and cartons, giant panettone tins etc. The sessions sparked many interesting conversations on various themes from litter to health and wellbeing, utility costs and local food to visiting local and national gardens. A participant said the sessions had helped combat social isolation after a bereavement. At the final session, the learners all wanted to continue sowing and growing which led to a plan to run monthly ”Grow and Chat” sessions at Moorlands Community Centre.
These are just a couple examples of some of the great work being carried out to support Southampton to reduce health inequalities across the City. However, there is still much to be done and the public health team have identified a number of key improvements:
- Champion and lead our workforce to develop a shared understanding of health inequalities.
- Continue to advocate on behalf of our residents to influence and improve the wider determinants of health in the city, including poverty.
- Grow momentum for the work to improve the impact that large organisations anchored within the city have.
- Review and continuously improve the equity of work through established processes such as health equity audit and health impact assessment. Who benefits and who doesn’t? Who has a good experience and who doesn’t? Commit to a new way of working with and alongside communities - a different relationship is good for us all.
What are we doing to tackle health inequalities?
When we’re safe and secure at home it can be hard to imagine how different life would be if we lost our home and became homeless.
This is because our home is so much more than a physical shelter. Home can be the place where we are happiest, a place we are loved for all our perfect imperfections, the place that evokes a sigh of relief when we walk through the door – whether it’s the welcome chaos of family life, the meow of the cat greeting you, the dog singing with delight at the sound of your key in the door – or perhaps our one place of stillness and silence, where we shut the world outside.
Sadly, this is not the same experience for everyone. For some, home can be a place of fear, apprehension, exploitation, hurt, anger or trauma – and as such, our experience of home and the conditions into which we are born, grow, work, live, and age - shape our daily lives. It is our place of reference, whether it’s a positive or negative experience, home is the place which influences who we are as a person, as a friend, sibling, partner, child or as a member of our wider community.
Without a safe and secure home, nothing else can fall into place.
Individuals and families across our shared communities who live with the trauma of a troubled homelife, or those who lose their home, face sometimes repeatedly significant disadvantage.
Did you know, across Hampshire and the Isle of Wight:
- Homelessness is not confined to people sleeping rough but also includes people in temporary accommodation, unsafe/insecure housing, sofa-surfing, sleeping in cars and tents and this broader problem of housing instability affects around 10,000 households across our footprint
- National evidence shows that homelessness drives demand for high-cost health interventions with increased rates of re-admissions and with individuals often falling into crisis conditions
- Around one in every 235 households are experiencing homelessness
- Some often experience significant life challenges and/or trauma, compromising their ability to lead fulfilling lives or sustain healthy relationships, their home and work. Support can focus on problems such as “what’s wrong with you” rather than a more person-led approach like “what matters to you?”
- Others fall into cycles of homelessness, enduring mental ill health, inpatient stays, and imprisonment. Their physical and mental health can be compromised by co-occurring drug and alcohol use. They can experience entrenched poverty, periods of rough sleeping, long term ill health/disability and hunger
- Data insight tells us that people are often discharged/released from services without care of their next step. People are released to No Fixed Abode (NFA) simply because they have arrived into services with no fixed address – only for the cycle of crisis, treatment, recovery to crisis to begin again. “In NFA, out NFA”
- The average age of an adult experiencing homelessness in our footprint is 37-years-old – nationally, the average age of dying whilst homeless is 45-years-old for men and 43-years-old for women
- As well as the human cost of losing your home, homelessness alone costs our system an additional £38m per year
The Integrated Care Board (ICB) has been exploring how it can use the home as a founding determinant of health and wellbeing, asking the question like “how is your housing situation helping or hindering your wellbeing, your health, your recovery?”
By recognising that health begins at home, we are unlocking capacity and resources moving from a position of purely treating the symptoms of people's lives, to the place where people live their life, keeping people safe and well at home and in turn decreasing demand on acute and emergency services, increasing bed/flow capacity, sustaining more vulnerable tenancies, and more.
Stepping Out:
Over the last three years, we have nurtured and built a collaborative style of working with system partners using the home as a common denominator of health and wellbeing – quite simply because without a home, nothing else can fall into place.
Working in collaboration with local councils and housing organisations, we have developed a “step out” housing model which enables people to be discharged from rehab and/or acute services into their own permanent home.
Working with our partners at Abri, a housing association based in the south of England, Southern Health NHS Foundation Trust and the Society of St James, a Southampton based charity supporting the homeless, we have brokered a growing pipeline. This initially started with 15 permanent homes, pepper potted around local communities enabling patients to “step out” of mental health rehab facilities – improving inpatient flow, reducing readmissions and reducing the need for out of area placements.
Feedback from staff say:
- Patients leave with feelings of joy and happiness
- Increased staff morale seeing people step out of the system into true independence
- Patients were able to be discharged an average of three months earlier than expected
- Achieving bed cost savings of £27K per person and reduced costs/cost avoidance with zero readmissionsl plus wider savings to the public purse
Early evaluation with residents finds there is improved optimism and hope for the future, sustained mental wellbeing and people are able to live settled, secure lives back in the local community. One resident said: “I have come on leaps and bounds from where I was a year ago and having my own flat has played a part in that. My flat feels secure and it's so nice to have my own home; it gives me a sense of wellbeing and being in control.”
Minding Every Gap
The Hampshire and Isle of Wight Integrated Care System is one of seven systems across the country to have been selected to take part in a national inclusion health learning project run by The King’s Fund.
The national project covers a number of traditionally excluded populations such as people experiencing homelessness, migrants, people with substance misuse and others, and our work to transform service/system transition and discharge points.
In a multi-sector collaboration between health, the Office of the Police and Crime Commissioner (OPCC), probation and prisons services, police, local authorities and housing partners and the Government Department for Levelling Up, Homes & Communities (DLUHC), our combined data tells us that insecure housing and homelessness is a key factor driving the health inequality and rates of reoffending.
Our data evidences we can make the most impact by focusing as a system on people with the following three characteristics:
- Poor mental health
- Previous contact with the criminal justice system
- At risk of homelessness
Working alongside Winchester prison (health and resettlement services inside the prison), we are beginning to tailor our collective approach in two local areas – the New Forest and Basingstoke and Deane – to ensure that people leave prison with housing support and ongoing health care in place. We recognise that we need to work in a more person-led trauma informed way to sustain engagement with people but also to wrap support around the individual – helping them step away from services.
At a neighbourhood level we plan to work alongside people with experience of these services to review support pathways – to understand what “good looks like,” whilst seeking consistent and common strands, ensuring we maximise impact of community and voluntary assets in local areas. Cutting duplication, making support easier to access and giving more opportunities for people to stay engaged.
The financial savings in preventing prison release into homelessness from Winchester prison alone we estimate to be in excess of £6m per year, but getting this right for the individual person is beyond priceless.
To find out more about the minding every gap programme Jackie Stevens, former Associate Director of Strategic Work Programmes, shared a blog post on the King’s Fund website. She talks in more detail about the programme and shares the real-life story from someone who is coming to the end of a four-year prison sentence and what impact this is having on their mental health.
Successful "minding every gap" programme highlighted at national conference

The successful work of the "minding every gap" programme and the impact it is having across Hampshire and Isle of Wight was highlighted at a national conference recently.
Our former Associate Director of Strategic Work Programmes, Jackie Stevens, was joined by colleagues from Southern Health NHS Foundation Trust, the Kings Fund and Groundswell, to attend the 2023 Pathways Conference to give an update on how we are tackling health inequalities across the system.
The title of the conference was “Making Integrated Services Work,” and so it was only natural to highlight, as one example, the incredible work the Minding Every Gap programme.
Jackie said: “It was a great privilege to be part of the Kings Fund, Pathways and Groundswell team at the Pathways Conference 2023 ‘making integrated services work.’ Together with my colleague, Jon Pritchard, we shared the challenges and more significantly the opportunities of integrated care systems.
“We shared some of the amazing work taking place across Hampshire and Isle of Wight on health inequalities using the home as a lens to wellbeing. As system partners, we all recognise the importance of having safe and secure housing as we go about our daily lives.”
Integrated Care Strategy
Our first Hampshire and Isle of Wight Integrated Care Strategy, developed by the Integrated Care Partnership, was launched in January 2023 and has a clear focus on tackling health inequalities. Read it here.